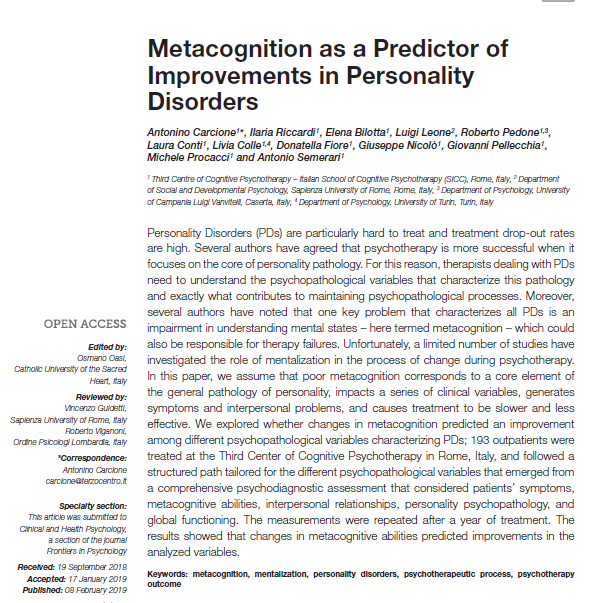
Personality Disorders (PDs) are particularly hard to treat and treatment drop-out rates are high. Several authors have agreed that psychotherapy is more successful when it focuses on the core of personality pathology. For this reason, therapists dealing with PDs need to understand the psychopathological variables that characterize this pathology and exactly what contributes to maintaining psychopathological processes. Moreover, several authors have noted that one key problem that characterizes all PDs is an impairment in understanding mental states – here termed metacognition – which could also be responsible for therapy failures. Unfortunately, a limited number of studies have investigated the role of mentalization in the process of change during psychotherapy.
In this paper, we assume that poor metacognition corresponds to a core element of the general pathology of personality, impacts a series of clinical variables, generates symptoms and interpersonal problems, and causes treatment to be slower and less effective. We explored whether changes in metacognition predicted an improvement among different psychopathological variables characterizing PDs; 193 outpatients were treated at the Third Center of Cognitive Psychotherapy in Rome, Italy, and followed a structured path tailored for the different psychopathological variables that emerged from a comprehensive psychodiagnostic assessment that considered patients’ symptoms, metacognitive abilities, interpersonal relationships, personality psychopathology, and global functioning. The measurements were repeated after a year of treatment. The results showed that changes in metacognitive abilities predicted improvements in the analyzed variables.